Yesterday in the New York Times, Jane Brody reminded us of the importance of cancer prevention when focusing on tobacco, the leading cause of cancer in the US and the world. This preventable cause of cancer continues to be marketed, but how do we quantify the prevention efforts that range from international agreements to counter tobacco, to state taxes that reduce smoking and support prevention programs, to local ordinances that help smokers quit or help prevent experimentation and addiction among our youth?
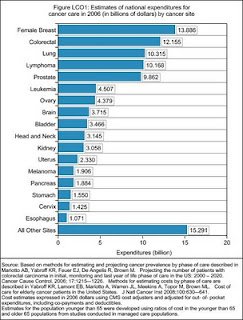
However we do the sums to add up the costs of our prevention efforts, they typically pale beside the resources committed to our focused research on discovery and development of new drugs and strategies to speed diagnosis and treatment of cancer. As of 2006, our national expenditures on cancer treatment exceeded 104 billion dollars, and with the number of cases of cancer diagnosed each expected to double over the next 40 years, these costs can only continue to rise. The full details of these costs broken down by cancer site are summarized in the NCI Cancer Trends Progress Report 1009/2010 (see link for details).
Importantly, an FDA advisory panel has recommended against continued use of a drug that shows little benefit among women with advanced stage breast cancer. As advocates at the meeting noted, false hope is not worth paying for. As we move to more personalized approaches to care that are determined by the genetic make up of the patient and the specific tumor being treated, we must continue to refine our approaches to determine which drugs are effective in which patients and carefully focus therapies accordingly.
But, as we spend more than 100 billion dollars on cancer treatment each year, can we refocus our attention on cancer prevention? Primary prevention can substantially reduce the cancer burden. Quitting smoking saves lives – never starting is even better (Kenfield, Stampfer et al. 2008; Kenfield, Wei et al. 2010). Decreases in smoking among men over the past 40 years have resulted in significant reductions in male lung cancers. But women have not caught up and the numbers continue to rise (Edwards, Ward et al. 2010). The value of prevention increases over time when messages remain constant or are refined as the science improves. The SunSmart prevention program in Australia highlights this approach and national success in countering the rise in melanoma. We however, continue to have increasing rates of melanoma in the US (Linos, Swetter et al. 2009). Our system rewards the development of “new approaches” rather than continuing to fund and use approaches that we already know work. In essence our priority for discovery overall application hinders progress in prevention. To bridge the gap from discovery to delivery and actual population health and wellness benefit, we need to fund programs that implement and sustain prevention that works. We also need to reward those who are committed to academic and local public health careers focusing on implementation and evaluation of programs that are known to work.
Contrasting prevention efforts with drug marketing is also helpful as it highlights sustained strategies to increase drug use (pharmaceutical detailing etc); whereas for prevention that is not focused on drugs our approaches are not as well coordinated and certainly not sustained. Take colorectal screening, for example, which can halve colon cancer mortality. We still have huge gaps in use of screening that persist even after access to care is covered through Medicare (Doubeni, Laiyemo et al. 2009; Doubeni, Laiyemo et al. 2010).
There are many successes of prevention over the years, but they get lost in the background, almost taken for granted once in place. On the other hand, new cases of cancer are diagnosed every day, pushing our systems of care to accommodate and ever increasing numbers of cancer patients. How do we balance these real world forces? Do you have ideas on how we might bring more political will to bear on sustaining prevention so we as a society reap the benefit?
References
Doubeni, C. A., A. O. Laiyemo, et al. (2009). “Socioeconomic and racial patterns of colorectal cancer screening among Medicare enrollees in 2000 to 2005.” Cancer Epidemiol Biomarkers Prev 18(8): 2170-2175.
Doubeni, C. A., A. O. Laiyemo, et al. (2010). “Primary care, economic barriers to health care, and use of colorectal cancer screening tests among medicare enrollees over time.” Ann Fam Med 8(4): 299-307.
Edwards, B. K., E. Ward, et al. (2010). “Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates.” Cancer 116(3): 544-573.
Kenfield, S. A., M. J. Stampfer, et al. (2008). “Smoking and smoking cessation in relation to mortality in women.” Jama 299(17): 2037-2047.
Kenfield, S. A., E. K. Wei, et al. (2010). “Burden of smoking on cause-specific mortality: application to the Nurses’ Health Study.” Tob Control 19(3): 248-254.
Linos, E., S. M. Swetter, et al. (2009). “Increasing burden of melanoma in the United States.” J Invest Dermatol 129(7): 1666-1674.